By YAN Fusheng (Staff Reporter)
Butterflies in the stomach. We’ve all felt it – that nervous sensation in the pit of your gut when you’re anxious or stressed. Turns out there’s scientific truth to this age-old idiom.
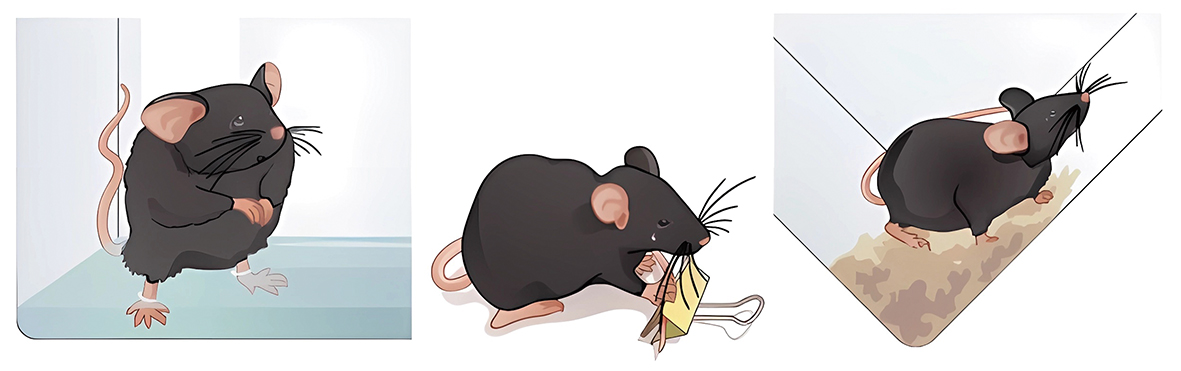
Male mice under chronic stress (living in a tilt cage and suffering from shallow water for 45 min and tail pinch for 15 min each day) are more likely to develop gastric dysfunction compared with unstressed ones. (Image by USTC)
Feeling butterflies in your stomach when nervous? There may be more science behind the saying than we realized.
In a new study published in Nature Metabolism on August 17, a research team led by Dr. ZHANG Zhi from the University of Science and Technology of China (USTC) and Dr. TAO Wenjuan from the Anhui Medical University in China have mapped a direct line of communication from the brain to the stomach that helps explain how stress can induce gastrointestinal issues.
Using advanced techniques, researchers traced a multi-step neural pathway starting from a brain area in mice called the dorsal raphe nucleus (DRN), which processes emotions and stress. Nerve fibers extend from here to the dorsal motor nucleus of the vagus (DMV), a region controlling the stomach and digestion.
The team also used miniaturized microscopes to spy on nerve cell activity deep in the mouse brain. They revealed that DRN neurons slowed down when the host is chronically stressed, firing fewer signals to the DMV.
Activating the pathway reversed poor appetite and sluggish digestion in stressed mice, demonstrating that the DRN-DMV-stomach axis directly regulates stress-induced stomach dysfunction. The pathway’s ability to regulate the functioning of stomach is hence bidirectionally verified.
These findings help explain the frequent gut complaints in patients with anxiety and depression. The study sheds light on the elusive brain-gut connection and shows that the DRN sends signals to control gastric activity, translating emotions into digestive effects. Stress seems to disrupt this communication, like a tightrope walker losing balance.
Could tweaking this circuit treat stress-related gut symptoms? Currently speculative, but an enticing prospect requiring further research.
Important questions remain before clinical relevance. For example, how exactly do acute versus chronic stresses change signaling? What causes circuit malfunction – anxieties, hormones, or both? Human studies are also essential.
There are societal implications to ponder as well. Stress-related gastrointestinal disorders are rising globally, incurring a heavy burden. Understanding its mechanisms is key for better prevention and treatment.
The intricate nerve circuitry linking emotions and digestion highlights the remarkable capabilities of the enteric nervous system – essentially a “second brain” within our gut.
The results underscore the potential for circuit-based therapies tuning the brain-gut axis. However, consciously considering the potential pros and cons of emerging neurotechnologies remains vital.
Reference
Dong, W. Y., Zhu, X., Tang, H. D., Huang, J. Y., Zhu, M. Y., Cheng, P. K., . . . Zhang, Z. (2023). Brain regulation of gastric dysfunction induced by stress. Nature Metabolism. doi:10.1038/s42255-023-00866-z

