By YAN Fusheng
Imagine a future where a single vaccine could protect you from a multitude of influenza strains, offering broad immunity with minimal risk. This vision is now closer to reality, thanks to a recent study that harnesses the power of cellular proteins to create a new generation of live attenuated vaccines that outsmart flu’s relentless mutations.
Every cell has a built-in cleanup crew called the ubiquitin-proteasome system (UPS). These ubiquitin tags act as a beacon, signaling the proteasome (the cell’s shredder) to dismantle the labeled protein into reusable building blocks. This natural shredder, in recently published research, is utilized to develop a ubiquitously applicable vaccine array against flus.
Led by Dr. SI Longlong from the Shenzhen Institutes of Advanced Technology (SIAT) under the Chinese Academy of Sciences, a group of researchers weaponized the UPS to disarm live flu viruses and turn them into vaccines.
In their paper published in Nature Microbiology on January 15, the team offers a systematic way to generate a library of PROTAR (PROteolysis-Targeting) vaccines that are both safe and highly effective, with the potential to protect against a wide range of influenza strains.
The Challenge of Influenza Vaccines
Flu viruses are RNA viruses armed with eight genetic segments. Their surface antigens—hemagglutinin (HA) and neuraminidase (NA)—mutate constantly (a process called antigenic drift) to evade the immunity of potential hosts. Unlike DNA viruses, their genome can undergo major evolutionary change with the entire gene segments swap between strains (antigenic shift), hence effectively becoming a new subtype.
Flus so novel, vaccines crumble—conventional vaccines chase the fleeting targets in vain. Derived from inactivated or weakened viruses from a predicted strain, traditional shots can only train host immunity on HA/NA combos prevailing months before and hence lag behind the viruses’ mutation. They often fail to provide complete matches with circulating strains, leading to suboptimal efficacy—like using last year’s map to navigate a mutating maze. The idea of converting circulating virus as a whole into attenuated, live vaccine is promising but fraught with safety concerns—risks unleashing the storm they aim to calm.
PROTAR Vaccines: Engineering Viral Self-destruction
Here’s the genius strategy: instead of chasing moving targets, PROTAR vaccines lock onto static ones—the evolutionarily conserved, less mutable proteins essential for viral survival. By selectively degrading these stable proteins within infected cells, PROTAR viruses are rendered replication-incompetent (hence, live-attenuated), preventing spread and cell infections. Proteasome-mediated degradation would flood the cell with viral protein fragments, which could be displayed on the cell surface to alert the immune system, triggering robust and broad-spectrum immunity.
But how do scientists ensure PROTAR viruses self-destruct before spreading?
The process begins with reverse genetics—a method to resurrect and reconstruct viruses from scratch in the lab by assembling their genetic components. Researchers use viral plasmids (circular double-stranded DNA) as customizable blueprints. For influenza, a segmented negative-sense RNA virus, eight plasmids encode each RNA segment, while four additional plasmids express viral polymerase proteins (PA, PB1, PB2) and nucleoprotein (NP)—the 12-plasmid system. When transfected into host cells, these plasmids orchestrate viral assembly via hijacking the host’s resources.
One plasmid encodes the M1 protein—a conserved scaffold essential for viral particle assembly. Without functional M1, viruses cannot exit host cells, making it an ideal target for designing PROTAR vaccines.
To ensure PROTAR vaccine’s safety, the team fused M1 to a proteasome-targeting degron (PTD), a molecular tag that recruits the cell’s ubiquitin-proteasome system, the built-in “protein shredder”. In human cells, E3 ubiquitin ligases recognize the PTD, ubiquitinate M1, and mark it for proteasomal destruction. This sabotages viral assembly, rendering PROTAR viruses harmless.
To mass-produce PROTAR vaccines, researchers engineered TEVp cells—specialized cell lines expressing tobacco etch virus protease (TEVp). In these cells, TEVp cleaves off the PTD tag from M1, allowing intact viruses to replicate safely in these cell factories from a petri dish. Harvested PROTAR viruses retain the PTD, ensuring self-destruction in human cells while serving as potent live-attenuated vaccines.
By targeting M1, PROTAR vaccines could induce immunity against diverse strains. Since M1’s structural role constrains its mutability, nearly all circulating influenza variants share nearly identical versions of this protein—a universal Achilles’ heel that can be targeted by PROTAR’s precision degradation.
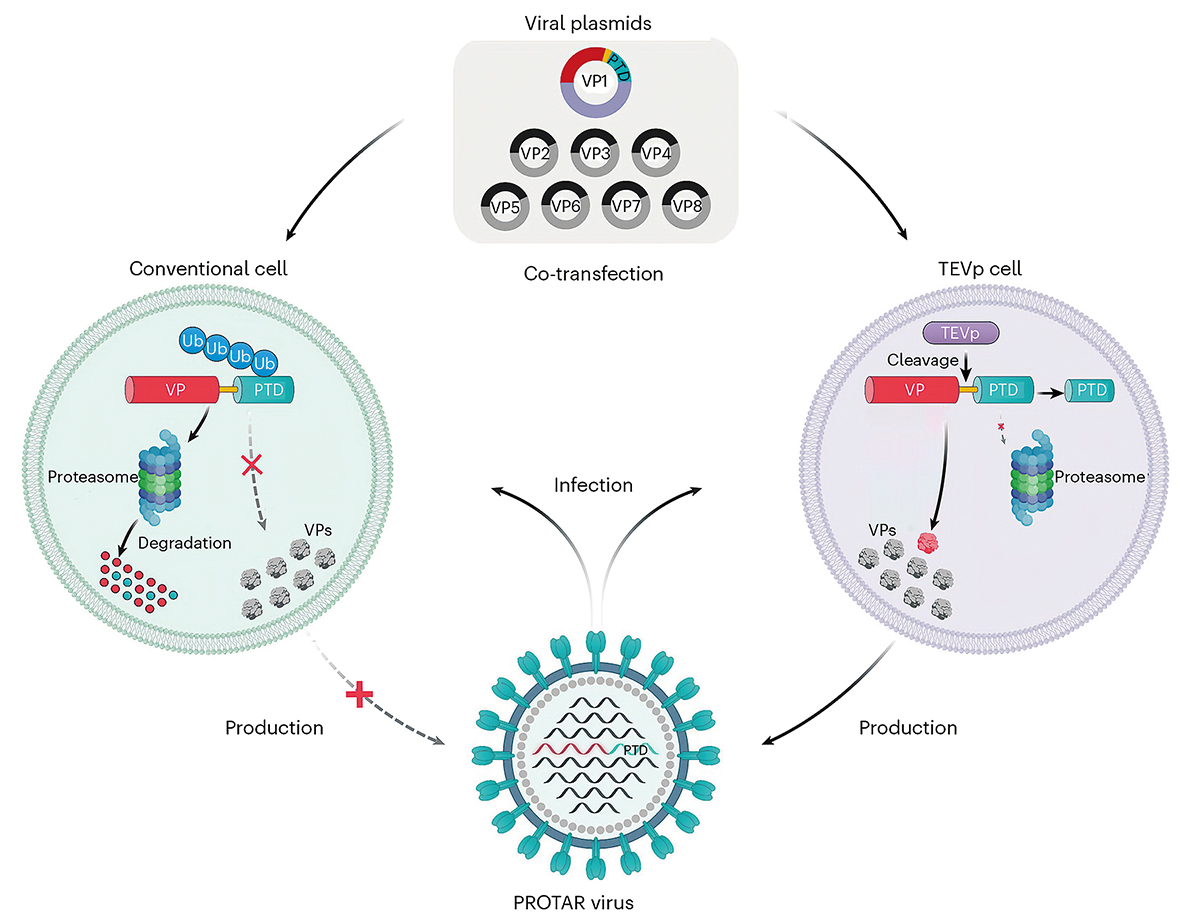
PROTAR vaccine: Engineering viral self-destruction in host cells (left) and vaccine production in a specialized cell line (right). Left: Viral proteins tagged with PTD are flagged by ubiquitin (Ub) for proteasomal destruction, blocking viral assembly and leading to live-attenuated vaccines. Right: TEVp (“molecular scissors”) removes PTD, allowing viral assembly. Harvested PROTAR viruses serve as live vaccines. VP, viral protein; Ub, ubiquitin; PTD, proteasome-targeting degron. (Graphic: SIAT)
Safety and Efficacy
The study shows that the PROTAR viruses were highly attenuated in human lung airway chips, an in vitro surrogate mimicking human lung tissue. While testing in mice, by day 3 after infection, PROTAR viruses were undetectable in mouse lung tissues. In contrast, the wild type (WT) virus replicated strongly. This shows that PROTAR viruses are significantly weakened in vivo, demonstrating PROTAR vaccine’s safety.
In mice, a single dose of PROTAR vaccine provided complete protection against both homologous and heterologous viral challenges, even in elderly mice and those with pre-existing flu immunity. These two groups are typically more challenging to protect effectively due to age-related immune decline (immunosenescence) and the presence of pre-existing antibodies that may interfere with new vaccine responses.
Flow cytometry analysis showed that PROTAR vaccines, which use PTD-mediated viral protein degradation, produced 2 to 10 times more viral peptide antigens compared to traditional vaccines, potentially explaining why PROTAR vaccines trigger stronger T-cell and B-cell immune responses.
The protective effects induced by PROTAR vaccine were also verified in ferrets, a valuable animal model that is more closely related to humans than mice are, specifically in the context of influenza infection, because ferrets are susceptible to influenza viruses and exhibit similar disease symptoms as humans. When challenged with a high dose of WT viruses three weeks after vaccination with PROTAR vaccine, no virus was detected in their nasal washes by day 3. This demonstrates the vaccine’s strong protection against infection.
These results suggest that PROTAR vaccines can induce strong and broad adaptive immune responses, which are crucial for long-lasting protection against influenza.
The team tested 22 different E3 ubiquitin ligases (an enzyme that marks specific proteins with ubiquitin chain, signaling their degradation), each with its own degron, to create a diverse library of PROTAR vaccines. For people with genetic quirks—like those lacking certain E3 ligases—PROTAR’s versatility allows scientists to handpick alternative ligases that compensate for these gaps.
Future Influenza Vaccine and Beyond
This study represents a significant advancement in vaccine development, offering a systematic and versatile approach to creating live attenuated vaccines. The PROTAR strategy could potentially be applied to other pathogens, opening new avenues for vaccine research.
However, as with any new vaccine technology, there are potential concerns, such as the possibility of viral escape from degradation or the impact of targeting specific E3 ubiquitin ligases in different populations. The researchers acknowledge these challenges and emphasize the need for further study to optimize vaccine candidates and ensure safety across diverse genetic backgrounds.
As the world continues to grapple with the ever-changing landscape of infectious diseases, this innovative approach to vaccine development offers hope for a more effective and adaptable solution to influenza and beyond.
Reference
Neumann, G. et al. (1999) Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl Acad. Sci. USA 96, 9345–9350.
Shen, J., Li, J., Shen, Q., et al. (2025) Proteolysis-targeting influenza vaccine strains induce broad-spectrum immunity and in vivo protection. Nature Microbiology. 10(2):431–447. doi:10.1038/s41564-024-01908-2

