Obsessive-Compulsive Disorder (OCD) is a debilitating and chronic disorder with a lifetime prevalence of near 1%, with up to 80% of those affected exhibiting symptom onset in childhood and adolescence. It is characterized as recurrent, intrusive thoughts (obsessions) and repetitive behaviors (compulsions), which heavily affects work and life of patients and causes large burden for family and society. Particularly, 30%~40% of OCD patients fail to respond adequately to the first-line treatments (i.e., medication and cognitive-behavioral therapies). Psychosurgical interventions, such as capsulotomy and cingulotomy, have been used as “last-resort” treatments for patients with treatment-refractory OCD. However, evidence of the neural circuit mechanisms through which therapeutic effects are achieved and what underlies response variability remains scarce.
A work published online on April 21, 2018 in Biological Psychiatry might have made some difference in this field. Titled “Dissociable Frontostriatal Connectivity: Mechanism and Predictor of the Clinical Efficacy of Capsulotomy in Obsessive-Compulsive Disorder,” this work was performed by Dr. WANG Zheng’s lab at the Institute of Neuroscience (ION), Chinese Academy of Sciences (CAS), and Dr. SUN Bomin’s team at Shanghai Jiao Tong University Medical School Affiliated Ruijin Hospital.
This work used resting-state fMRI (functional magnetic resonance imaging) to investigate neural mechanism and response variability underlying neurosurgical interventions for severe OCD. The results indicated that two dissociable frontostriatal circuits might underlie the mechanism and the predictor of the clinical efficacy of capsulotomy in severe OCD, respectively. This work might improve our understanding of network effects underlying a targeted surgical therapy, and holds potentials for using a functional connectivity marker to guide treatment decisions.
To address the above-mentioned questions, researchers used the resting-state functional connectivity approach to examine alterations in frontostriatal circuitry before and after capsulotomy (Fig. A illustrates the surgical target and seed regions). In OCD patients, functional connectivity between ventral striatum and dorsal anterior cingulate cortex (dACC) was reduced after the surgical procedure. More importantly, the change in connectivity significantly correlated with clinical improvement. To explore the response predictors of capsulotomy for OCD patients, the preoperative frontostriatal connectivity that could differentiate responders and non-responders were identified firstly. Then, a linear regression model was applied between the strength of identified connectivity and changes in Y-BOCS scores. The results showed that preoperative connectivity between dorsal caudate and dACC predicted changes in Y-BOCS score, which was further validated in an independent group of patients (Fig. B). Collectively, this study demonstrated that restoration of ventral frontostriatal connectivity was associated with clinical improvement in severe OCD, suggesting a therapeutic mechanism of capsulotomy. Moreover, preoperative variations in dorsal frontostriatal connectivity predicted clinical response, which may offer a predictor of treatment outcome.
This work was completed by Dr. YIN Dazhi and Mr. ZHANG Chencheng, under the supervision of Profs. WANG Zheng and SUN Bomin, and funded by the National Key R&D Program of China, the Strategic Priority Research Program (B) of CAS, grants from THE National Natural Science Foundation of China, the Shanghai Jiao Tong University School of Medicine–Institute of Neuroscience (SHSMU-ION) Research Center for Brain Disorders, and the Natural Science Foundation and Major Basic Research Program of Shanghai. The authors thank JIANG Qinying and YU Wenwen for their assistance in data collection.
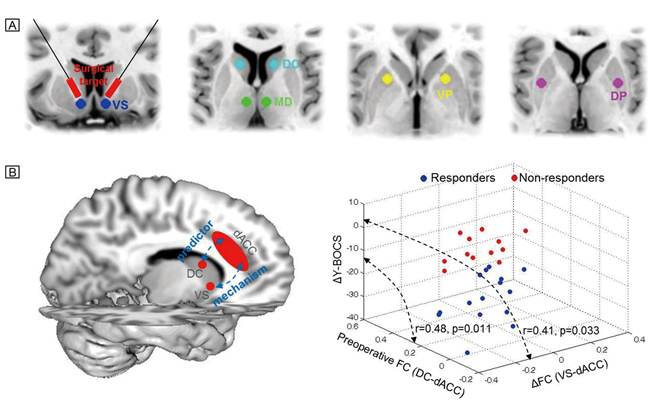
A) Illustration of the surgical target and seed regions.
B) Two dissociable frontostriatal circuits underlie the mechanism and the predictor of the clinical efficacy of capsulotomy in severe OCD, respectively.

