By YAN Fusheng (Staff Reporter)
Targeted cancer drugs might fail to reach their destination due to the resistance from the tumors’ defense system. Now, researchers have found a way to infiltrate these defense barriers by leveraging the immune system to open the gate.
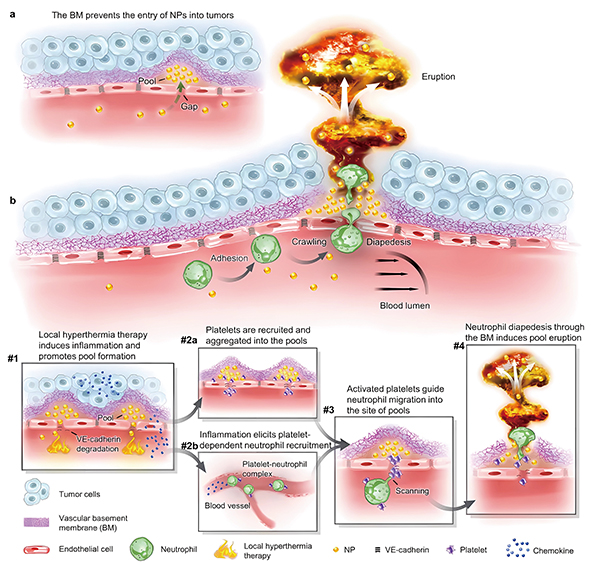
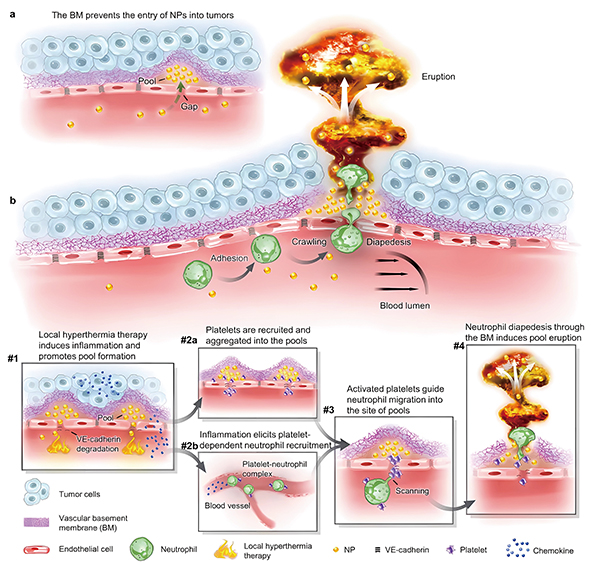
Local hyperthermia therapy increases the number of pools around tumor vessels that can take nanoparticles. Then, the recruited neutrophils open the basement membrane barrier during infiltration, releasing trapped nanoparticles from the pools in a series of repeatable “bursts” that penetrate deeply and efficiently into the tumor. (Image by USTC)
For years, scientists have sought to develop nanoparticle-based drugs that can precisely target and eliminate cancer cells. But a major roadblock has stumped even the brightest minds: the tumor’s biological barriers prevent nanoparticles from reaching their targets. Now, a joint research team from the University of Science and Technology of China (USTC) and the National University of Singapore has found an innovative way to overcome these obstacles by enlisting the help of the immune system. Their findings, published in Nature Nanotechnology on September 14, may contribute to developing more effective antitumor therapies.
Imagine an armored convoy trying to deliver supplies to soldiers on the frontlines. But between the convoy and its destination lies a nearly impenetrable fortress wall. Try as they might, the supply trucks cannot get through. Likewise, when administered intravenously, therapeutic nanoparticles become trapped behind tissue barriers surrounding tumors. Specifically, nanoparticles accumulate inside void spaces between blood vessels and an underlying basement membrane – a thin, fibrous envelope sheathing the vessels. As a result, these therapeutic nanoparticles fail to function as they were meant to.
The new study first demonstrated this barrier’s pivotal role in obstructing nanoparticle delivery. Using advanced intravital microscopy techniques, the researchers imaged the phenomenon in mouse models of breast cancer, colorectal cancer and pancreatic cancer. After injecting fluorescent nanoparticles intravenously, they watched in real time as the particles aggregated into voids between vessel endothelial cells and the enveloping basement membrane. Try as they might, the trapped nanoparticles could not breach this barrier.
It’s like the nanoparticles were waiting at the gates but could not enter the castle.
The study, thankfully, solved the problem by leveraging the immune system to literally blast through this barrier and ferry nanoparticles into the depths of the tumor.
To “open the gate,” the researchers applied mild heat therapy. They discovered this attracts platelets – disk-shaped cell fragments involved in blood clotting. Acting like emergency responders to the heat-induced inflammation, platelets rushed to the void spaces where nanoparticles were stuck.
The platelets, in turn, summoned immune cells called neutrophils, white blood cells that travel to sites of infection or injury. When neutrophils arrive at areas of tissue damage, they normally crawl through walls of blood vessels to combat pathogens. But in this case, the researchers found they performed a different function. Acting like breach teams at the fortress walls, these cells bored holes in the membrane barricade at sites of trapped nanoparticle pools.
Attracted by molecular signals from platelets, neutrophils directly headed to the nanoparticle pool sites. Upon arrival, they breached the basement membrane barrier by poking small holes. Pressurized nanoparticles then erupted through these openings, gaining direct access to the tumor.
Using this strategy, the researchers showed they could enhance nanoparticle delivery to tumors in mouse models of breast cancer, colon cancer and pancreatic cancer. Treatment with a nanoparticle drug formulation called liposomal doxorubicin, once administered along with this strategy, caused enhanced tumor shrinkage compared to administered alone.
These findings revealed an overlooked barrier posed by the tumor vascular basement membrane. By enlisting the help of the immune system, the team engineered a strategy to overcome this barrier and boost the delivery of nanomedicine payloads.
The study demonstrates a groundbreaking approach that could vastly improve treatment outcomes for cancer patients. By harnessing the immune system’s power, scientists may finally have a way to defeat biological barriers that have long obstructed nanoparticle delivery to tumors. This could usher in a new era of precise, targeted cancer therapy.

